Gaining Ground Against Alzheimer’s
Editor’s Note: This feature was originally published in the summer 2025 print edition of NEXT. To view a PDF of the full issue, visit our publications page.
By Paul Brockwell Jr., MCV Foundation
Photos by Daniel Sangjib Min, MCV Foundation
Millions of families say a long and gut-wrenching goodbye to a loved one with Alzheimer’s disease.
Over time, the brain of the once vibrant person they know and love will succumb to the telltale deterioration. People whose lives lit up rooms will fade into unrecognizable versions of themselves. They may even forget the ones they love the most.
What scientists know today is that the disease appears strongly linked to inflammation responses in the brain that cause a build-up of protein clumps and tangles that accumulate over time and begin to disrupt healthy function between nerve cells. The disease, which can progress for years before outward behavioral symptoms develop, robs its victims of the very thoughts and memories that make up their identity. The good days and bad days are marked by the ebb and flow of emotional suffering that some families and caregivers experience.
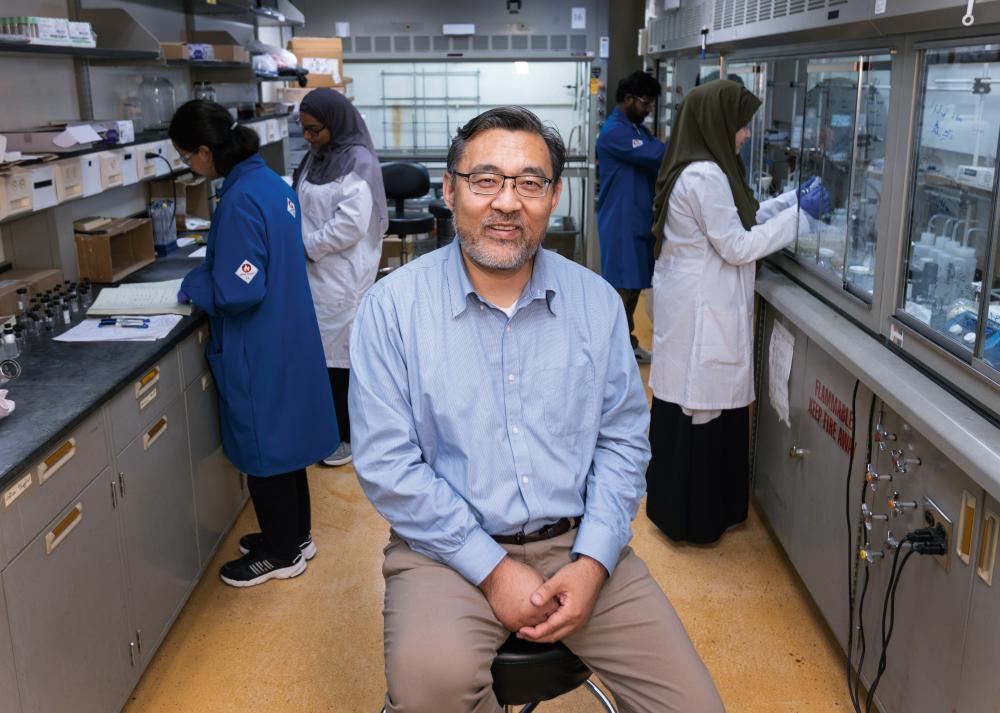
Shijun Zhang, Ph.D., knows that anguish well. He witnessed it when hearing heartbreaking stories from families of patients while serving as a member of the board of the Greater Richmond Chapter Alzheimer’s Association. And he’s lived it in the two years since his mother-in-law received a dementia diagnosis.
Since 2008, that agony has helped fuel his work to engineer new drugs that stop the vicious cycle of inflammation, and he’s more optimistic than ever for a breakthrough that can give hope to both patients and families whose lives are often upended by the demands of caring for their loved one around the clock.
“There is a huge burden on caregivers,” said Dr. Zhang, professor and graduate program director in the VCU School of Pharmacy’s Department of Medicinal Chemistry. “We need to have something that is more effective not only at treating this disease, but also to help reduce the emotional and financial burden on the caregivers.”
Nearly 7 million Americans are living with Alzheimer’s disease today. By 2050, that number is expected to double to 14 million, according to the Centers for Disease Control and Prevention. Globally that patient population is around 55 million, and it’s expected to double every 20 years, according to Alzheimer’s Disease International. By their estimate, someone around the world develops dementia every 3 seconds.
We have reached the third generation of molecules and in some of them, the potency is very promising. With some of them we have observed significant suppression of the targeted inflammasome.
Shijun Zhang, Ph.D., professor and graduate program director, VCU School of Pharmacy’s Department of Medicinal Chemistry
The need for a medical breakthrough has never been more urgent. In 2021, the FDA approved aducanumab, the first new drug in nearly two decades to treat Alzheimer’s. But that decision was contentious, and the results have been marginal. Since then, the FDA has approved additional drugs including lecanemab in 2023 and donanemab in 2024. The approved treatments are monoclonal antibodies, or lab-produced proteins designed to mirror the body’s immune response. In Alzheimer’s drugs, the antibodies are designed to target amyloid deposits, a key pathology of the disease long suspected of playing a role in its development.
The available treatments themselves are incredibly costly, and they require additional costs for regular follow-up MRI imaging to monitor risks such as hemorrhaging and cerebral edema. Monoclonal antibody treatments for Alzheimer’s have only achieved between 27% and 30% improvement in patients when it comes to regaining cognitive function, said Dr. Zhang.
“We need something more effective, and I think a small molecule solution could be a preferred way to pursue treatments,” he said.
Tucked in a lab space in downtown Richmond, Va., he’s been making remarkable progress on that challenge by building and testing small molecules that could be the key to disabling the body’s internal alarm system that drives chronic inflammation.
FROM BASIC SCIENCE TO NEW TREATMENTS
Scientific consensus recognizes that neuroinflammation plays a role in the development and progression of Alzheimer’s disease. To address that pathology, Dr. Zhang and his lab have focused on engineering molecules that can help tamp down inflammation associated with Alzheimer’s disease. In particular, he has been working to identify drugs that target a particular inflammasome, NLRP3, a group of proteins that behave like a home security system for the body’s innate immune response. When NLRP3 detects danger signals in a cell, it triggers additional inflammation response through signaling.
Delivery of New Treatments
It’s a challenge to design drugs with the right qualities of movement through the body that can ensure the medicine can get to the area of the body where it’s most needed. Solving that challenge can make the difference between a treatment that requires regular injections for delivery or oral tablets. From a patient perspective, a tablet taken orally presents fewer barriers to access and compliance with a treatment than more involved delivery mechanisms.
The type of small molecules that Dr. Zhang is testing would inhibit the inflammasome response in the brain. The active agents in this potential treatment are small molecules that Dr. Zhang and his team, including research assistant professor Yiming Xu, Ph.D., design and build at the bench through an iterative process, synthesizing and testing how efficient and effective the candidates are for suppressing the inflammasome. From there, additional testing and imaging is done in animal models to ensure effectiveness. One of the agents he has developed shows great promise as a potential treatment and has achieved more than 50% suppression of the target inflammasome at a dose of 5 mg/kg in preclinical animal models.
Some of the biggest challenges for drug discovery are finding solutions that can cross the blood-brain barrier, a selective semi-permeable membrane that allows cerebral blood vessels to regulate molecule and ion movement between the blood and the brain. It’s a challenge to design drugs with the right qualities of movement through the body, or pharmacokinetic properties, that can ensure the medicine can get to the area of the body where it’s most needed. Solving that challenge can make the difference between a treatment that requires regular injections for delivery or oral tablets. From a patient perspective, a tablet taken orally presents fewer barriers to access and compliance with a treatment than more involved delivery mechanisms.
“We have reached the third generation of molecules and, in some of them, the potency is very promising,” Dr. Zhang said. “With some of them we have observed significant suppression of the targeted inflammasome by the molecules, which is really quite good. We’ve also been able to achieve brain penetration and are reaching the point for a suitable oral pharmacokinetic property, which will be critical for the clinical studies.”
In a separate research project, Dr. Zhang’s team has been exploring ways to address mitochondrial dysfunction, another source behind Alzheimer’s. When mitochondria, the powerhouses of cells, are not functioning normally, they are linked to oxidative stress and inflammatory responses as well as other pathologies of Alzheimer’s. The theory is that by helping address mitochondrial dysfunction as a driver of multiple Alzheimer’s pathologies, treatments could reduce root causes to provide more effective treatments for Alzheimer’s and other dementia types.

“Initially when we started these two projects, they were unrelated,” Dr. Zhang said. “But with further studies, we realized these are not two isolated targets, which has made this research more exciting. They are actually closely interconnected.”
Dr. Zhang and his team have connected the two projects to the same common treatment pathway, which is regulating the immune responses. He believes that ultimately researchers may discover that combining effective therapies may be the key to a long-term treatment, a theory that underlies his work targeting both the inflammasome and the mitochondrial dysfunction in order to provide a one-two punch toward addressing the pathology of Alzheimer’s disease development.
IMAGING PROJECT PROVIDES KEY INSIGHTS
Developing a drug is its own iterative process, but so is the challenge of proving the efficacy of potential candidates. In 2022 and 2023, Dr. Zhang and his team received grants from the Commonwealth of Virginia’s Center on Aging, National Institute on Aging and the Alzheimer’s Drug Discovery Foundation to build and test radiotracers for using positron emission tomography (PET) by targeting the NLRP3 inflammasome to prove the efficacy of future drug candidates. The new PET imaging tools are also aimed at identifying good biomarkers and ways of imaging neuroinflammation.
“The PET imagining tools will help us test whether neuroinflammation is a good biomarker for Alzheimer’s disease,” Dr. Zhang explained. “They also will make it possible to image the progression of neuroinflammation. Not only would these tracers help us in the future clinical evaluation of potential drug candidates, but they also can become useful diagnostics in the future when neuroinflammation is accepted as a biomarker.”
Neuroinflammation likely begins much earlier than the plaque and tangle pathology associated with advanced disease. His hope is that some combination of therapies and the PET imaging could help physicians provide the best available interventions earlier for those at risk of developing severe disease. Emerging research suggests that the disease can begin developing 20 years before symptoms become clear in patients.
The imaging and diagnostic project is the third leg of the stool when it comes to Dr. Zhang’s research. He said progress is possible when combining the imaging with his projects aimed at stopping inflammation by inhibiting the NLRP3 protein as well as taming mitochondrial dysfunction as a driver of other pathologies linked to disease progression.
WHAT’S NEXT?
Dr. Zhang and his team are working toward the goal of conducting enabling studies to investigate a new drug next year. Enabling studies are a critical step that bridges the gap between preclinical and clinical research. During this phase, Dr. Zhang and his team will seek to prove both the efficacy and safety of potential drug candidates. Once his lab can prove the effectiveness of a drug candidate and that the drug itself is not harmful or toxic in preclinical animal models, investigatory phases involving clinical trials will become possible.
“We never imagined we could end up where we are now,” Dr. Zhang said. “With the support of the university and these grants, we can do some real drug discovery and maintain full-speed ahead on identifying drug candidates with good pharmacokinetic properties and efficacy.”
In February, the team received commercialization funding from VCU TechTransfer and Ventures, which will help advance their research. While Dr. Zhang remains focused on the Alzheimer’s drug development project, he’s also quick to point out that inhibiting the NLRP3 inflammasome has exciting potential application to other disorders associated with inflammation, from chronic pain to autoimmune disorders and chronic gastrointestinal diseases.
“The commercialization funds were a great addition to this project and will allow us to pursue pharmacokinetic studies to help speed the process,” Dr. Zhang said. “It’s also exciting to see how this research could grow to have an impact on other chronic inflammation-driven diseases.”
If you are interested in learning more about how to support Dr. Zhang’s research on Alzheimer’s disease, please contact Louie Correa, senior director of development at VCU School of Pharmacy, at 804-828-3016 or lacorrea@vcu.edu.
Stay Connected
Sign up to be inspired by stories of incredible innovation through our publication mailing list.