Rethinking Painkillers
Editor’s Note: This feature was originally published in the summer 2025 print edition of NEXT. To view a PDF of the full issue, visit our publications page.
By Olivia Trani, VCU Health
People don’t ask to descend into opioid addiction. They don’t ask for the physical dependence — the cravings and the sweating. They don’t ask for it to control and affect every moment of their lives.
It could happen to any of us.
Dispensed for prescriptions approximately 125 million times in 2023 to manage chronic pain or pain following surgery, physical trauma, and cancer diagnosis, opioids do work — but their risks are significant.
In 2023, nearly 8.6 million Americans reported misusing prescription opioids in the previous year, and from 1999 to 2022, approximately 294,000 people died from overdoses involving prescription opioids. Compounding the problem is that in many cases, misuse of prescriptions leads to use of illegal drugs such as heroin and fentanyl.
So, as more than 50 million people in the U.S. suffer from chronic pain and millions more face surgeries, trauma and cancer diagnoses, what is the safe answer? Is there a safe answer?
The answer is that a reliable, nonaddictive drug to ease suffering remains out of reach. However, researchers at VCU are leading successful pursuits to create new, nonaddictive painkilling agents and re-engineer available treatments for opioid use disorder that work better.
Our process has really been a bottom-up discovery. This research originally started with understanding the inhibitor at the molecular level, while this new study aimed to better understand how the inhibitor has an impact at the cellular and behavioral levels.
Aron Lichtman, Ph.D., professor, VCU School of Medicine’s Department of Pharmacology and Toxicology
They are working with teams from the University of Texas at Austin and the University of Virginia to develop a novel drug candidate for treating chronic pain more safely that works by turning off the body’s inflammation. In their most recent study, published in Proceedings of the National Academy of Sciences, the researchers found that the drug candidate was able to effectively trick immune systems in such a way as to shut off an inflammatory response, thereby alleviating pain. While this research is currently at the preclinical stage, the ultimate goal is to make an effective and targeted treatment for people suffering from chronic pain.
Promising Drug Candidate Sparks Collaboration

Immune cells in the human body produce compounds called endocannabinoids which, among other things, regulate inflammation. In a healthy person, inflammation is a process that helps the body heal from infections or injuries. But the downside is that it also causes swelling and buildup of tissue that presses on nerve endings and causes persistent pain.
“When the endocannabinoids in our bodies cause inflammation, our nerves become sensitized. They react more rapidly with less stimulation than is normally needed. This causes things that normally wouldn’t hurt to suddenly become extremely painful, similar to how we feel when we have a bad sunburn,” said Aron Lichtman, Ph.D., a professor in the VCU School of Medicine’s Department of Pharmacology and Toxicology.
In this study, the researchers analyzed an inhibitor called KT109 that blocks the activity of an endocannabinoid-producing enzyme in immune cells called DAGLß.
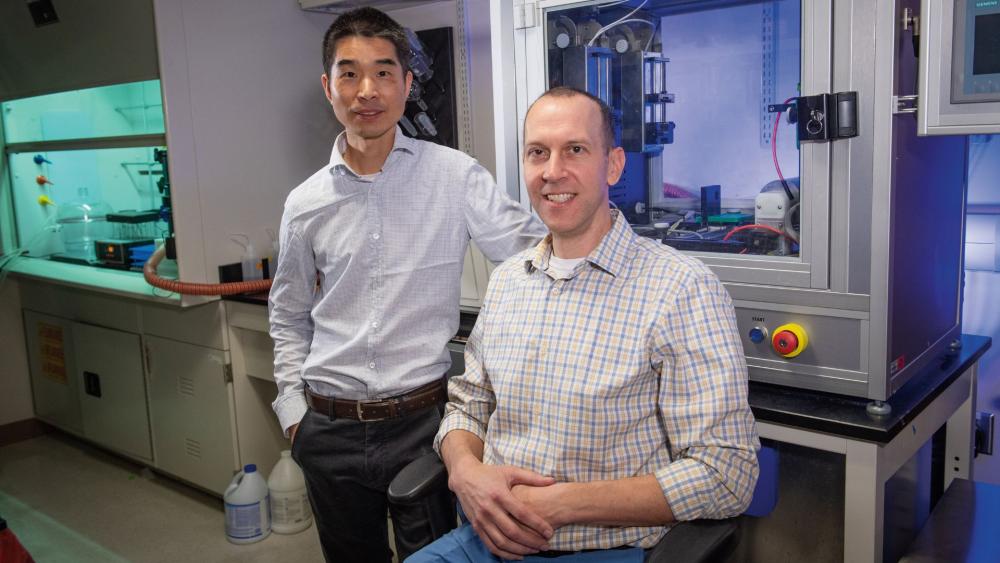
Ken Hsu, Ph.D., an associate professor in the Department of Chemistry at UT Austin, developed the inhibitor as a postdoctoral fellow at The Scripps Research Institute. He has since fostered a long-term collaboration with Dr. Lichtman and Hamid Akbarali, Ph.D., also a professor in VCU’s Department of Pharmacology and Toxicology, to better understand how inhibiting DAGLß reduces inflammation and the associated pain.

Dr. Akbarali’s expertise is investigating how inflammation impacts the nervous system at the cellular level. His research team examined how the drug candidate interfered with pain-transmitting neurons in mouse models.
“In our lab, we look at the speed and strength of the pain signals that neurons send to the brain, and for this particular project, we analyzed how the drug candidate weakened these signals as they traveled through the nervous system,” he said.
Dr. Lichtman’s research team focused on understanding how these cellular processes then impact the behavior and function of chronic pain in animal models.
“Our process has really been a bottom-up discovery,” Dr. Lichtman said. “This research originally started with understanding the inhibitor at the molecular level, while this new study aimed to better understand how the inhibitor has an impact at the cellular and behavioral levels.”
UNCOVERING THE PATHWAY TO PAIN RELIEF
Previous work demonstrated how KT109 controls inflammation via inhibiting endocannabinoids and prostaglandins, which are a type of lipid, or fatty acid, that plays a significant role in pain perception by modulating the activity of receptors in the sensory nerve endings that detect pain. But in this latest study, the researchers were surprised to discover that KT109 also controls inflammation through an additional pathway, which helps explain why the inhibitor is effective in treating different types of pain.
“When you inhibit DAGLß, your immune cells are tricked into thinking they are starving,” Dr. Hsu said. “Changes in energy metabolism in the immune system can turn off inflammatory signaling and be effective in pain management.” One example is the drug metformin, which is commonly used to treat diabetes but also has been found effective in treating pain.
The team’s inhibitor targets DAGLß, which is mainly present and active in immune cells, thereby avoiding any unnecessary reaction with other cells that might lead to side effects.
“You’re going to affect these pathways where it matters, where the inflammation is happening,” Dr. Hsu said.
The researchers don’t believe this drug inhibitor acts in the brain, thereby avoiding the potential alteration of reward pathways in the brain that might lead to substance abuse.
The research team has so far only studied the effects of the inhibitor through injection, but the goal is to develop a pill that can be swallowed. To avoid internal toxicity, the researchers will aim to refine the chemistry and reduce the number of times the medicine needs to be taken while maintaining the same pain-easing effect.
The findings are helpful for pharmaceutical companies considering the development of medicines that target DAGLß in people experiencing chronic pain.
RE-ENGINEERING TREATMENTS FOR OPIOID USE DISORDER
As the U.S. continues to grapple with the unrelenting opioid crisis, researchers at VCU have also reformulated an opioid use disorder medication in a way that could extend its therapeutic effects. With a new formulation of one drug, they hope to offer a longer-lasting therapy for patients with opioid use disorder that addresses long-term challenges around treatment access and compliance.
In 2023, more than 150 people died every day on average from opioid overdose in the U.S., according to the Centers for Disease Control and Prevention. A number of medications help curb opioid addiction, but several barriers can interfere with a patient’s path to recovery, such as strict regulations, adverse side effects and limited access to treatment clinics.
In hope of providing more treatment options for opioid use disorder, the VCU research team reworked levo-alpha-acetylmethadol, also known as LAAM, a metabolite of a previous FDA-approved opiate dependence medication, into a new formulation that could be used to help patients with opioid addiction.
Their latest study, published in the Journal of Controlled Release, showed that the reformulated medication significantly reduced opioid use and withdrawal symptoms in animal models. The researchers say these findings have promising implications for ultimately expanding the range of medicinal therapies available for treating opioid addiction.
“There is an urgent need to develop more therapeutic strategies for enhancing the effectiveness of our interventions and the overall well-being of patients with opioid use disorder. Our goal is to give physicians another tool in their toolbox to help patients overcome addiction,” said Qingguo Xu, Ph.D., an associate professor in the VCU School of Pharmacy’s Department of Pharmaceutics. He co-led the new study with Matthew Banks, Ph.D., a professor in the VCU School of Medicine’s Department of Pharmacology and Toxicology.
There are currently three FDA-approved medications used to treat opioid use disorder: methadone, buprenorphine and naltrexone. Despite their effectiveness in helping patients curb addiction, barriers to access and other challenges persist.
“Part of the issue is that each of these medications comes with their own set of regulatory hurdles. In particular, methadone is very effective at decreasing illicit drug-taking behavior, but there are a lot of regulatory restrictions and stigma around its use,” Dr. Banks said. “Another challenge is that some patients are unresponsive to the current medications or experience undesirable side effects.”
“Some patients also have a hard time managing the dose requirements of the current medications,” Dr. Xu added. “Methadone treatment requires daily visits to an approved methadone clinic, which can be a huge burden for patients, especially if they live in rural areas with limited access to clinics. Since the pandemic, government officials have been working to loosen those restrictions.”
Previous research had shown LAAM was more effective than methadone in suppressing opioid use, but it was taken off the market in 2003 due to concerns about cardiac effects and declining sales after buprenorphine’s introduction as a prescription treatment. Drs. Xu and Banks saw an opportunity to reformulate LAAM to address safety concerns while also making treatment more accessible for patients.
The team’s research findings have demonstrated their new formulation of the medication, which they call nor-LAAM, could be a safer, more potent alternative to LAAM and existing drugs. Their goal is to give pharmaceutical companies a reason to bring back the medication as an additional option for reducing opioid cravings and preventing relapse. In this new formulation, the researchers also developed a novel drug-loading system that packs a high dose of nor-LAAM into biodegradable microparticles, which in turn releases a steady level of medication over a long period of time. While current medications for opioid use disorder often require daily doses, nor-LAAM is designed to be taken once a month, or potentially even less frequently.
“This is an important benefit since reducing the frequency of doses can make it easier for patients to comply with their treatment plans,” Dr. Banks said.
He and Dr. Xu have since been leading preclinical studies to better understand nor-LAAM’s potential for treating opioid use disorder. In their latest study, the researchers examined the behavior of fentanyl-dependent rodents when treated with either nor-LAAM or a placebo. They specifically looked into how the medication impacted the subjects’ preferences when given the option to either self-administer fentanyl or receive food.
Their study revealed that subjects treated with nor-LAAM significantly reduced their preference for fentanyl over food over the course of four weeks. Additionally, subjects treated with nor-LAAM exhibited fewer signs of opioid withdrawal over time.
While this project is still in the preliminary stages and it may be a few more years until this medication is ready for human clinical trials, the researchers say these findings give promising insights into nor-LAAM’s potential as a long-acting strategy for treating opioid addiction. Looking ahead, Drs. Xu and Banks will continue to develop nor-LAAM formulations and assess its effectiveness for therapeutic use.
“We hope that expanding the medicinal options for opioid use disorder helps with increasing patient retention to their treatments, gives them a better chance to overcome addiction and ultimately gives them back their lives,” Dr. Xu said.
The Next Generation
VCU is committed to training future leaders who can help end addiction.
The project to develop nonaddictive painkillers has received significant support from the Central Virginia Center on Drug Abuse Research, an interdisciplinary research center based at VCU that is focused on addiction to opioids and other drugs of abuse.
Fueled by a $6.8 million grant from the National Institute on Drug Abuse, the center provides funds and resources to advance promising research aimed at addressing addiction. Drs. Lichtman and Akbarali credit this grant with helping VCU be a leader in training the next generation of scientists to tackle drug abuse.
At VCU, students and trainees are given opportunities to join cutting-edge projects that build their knowledge on addiction research and other subjects. Many of the graduate students and postdoctoral researchers who contributed to this study are funded through the NIDA grant. VCU’s Department of Pharmacology and Toxicology initially secured the federal grant in 1976 to provide tuition, equipment and supplies to those training to be addiction researchers. The grant has been renewed every five years ever since, providing roughly $24 million in support to more than 600 students and trainees over the past 50 years.
“Our studies benefit from student involvement because they are the conduits of research and collaboration,” Dr. Lichtman added. “They are the ones actually at the bench doing this important work.”
In recent years, the university has expanded learning opportunities for students. In 2020, Omar Abubaker, D.M.D., Ph.D., made a lead gift to establish the Adam Abubaker Memorial Lectureship at the VCU School of Medicine. Dr. Abubaker, who holds the S. Elmer Bear Chair in Oral and Maxillofacial Surgery at the VCU School of Dentistry, wanted the lectureship to honor the memory of his son, Adam, who died from an opioid overdose in 2014.
The lectureship provides students in medicine and dentistry with opportunities to learn from national experts in addiction medicine on topics including prevention, treatment, community health, and understanding the science of addiction and substance use disorders.
“No parent should have to endure the hardship of a loss this great,” Dr. Abubaker said. “Doctors, including myself, were part of this opioid epidemic. I have made it my personal mission to be a part of the solution and to educate other health care providers on the dangers that opioid prescriptions pose and safe prescribing practices.”
If you would like to support addiction research on the MCV Campus, please contact Nate Bick, executive director of development in the Office of Medical Philanthropy and Alumni Relations, at 804-827-0387 or ngbick@vcu.edu.
Health. The Greatest Gift for All
Support incredible research at VCU and help train future health care leaders.