Warmth & Compassion

Editor’s Note: This story originally appeared in the winter 2023 issue of NEXT magazine. Our online version includes more stories about innovative research happening on the MCV Campus.
By Paul Brockwell Jr. and Danielle Pierce
The cool, blue and white hues of a large wintry painting are among the first things that visitors see when entering the eighth-floor burn unit at VCU Medical Center’s Critical Care Hospital. The choice was intentional: a piece with calming colors that are the opposite of fire and heat.
Sending a message through artwork is among the many details that the Evans-Haynes Burn Center has carefully managed in order to create a best-in-class center for treating patients with severe burns. Evans-Haynes is not only the oldest civilian burn unit in the country, it is also one of the best. It’s the only burn center in Virginia to be verified four times by the American Burn Association, whose rigorous evaluation process ensures continuous improvement and a growth mindset among the team. It’s worth noting that VCU Health’s burn center predates by 20 years the establishment of the American Burn Association, a professional organization dedicated to improving the lives of burn patients. It offers national verification based on patient safety and outcomes along with a commitment to innovation and research.
“Our patients get everything they need right here under one roof — pain team, therapists, nursing staff, reconstructive and plastic surgeons, burn-specific anesthesia and doctors whose care and expertise complement each other,” said Michael Feldman, M.D., the burn center’s medical director and the B.W. Haynes Jr., M.D., Endowed Professor at the VCU School of Medicine. “I think that’s part of what makes this burn center special — we offer the full gamut of what our patients need.”

Each year, the center — with 16 total beds — treats 600 to 650 pediatric and adult patients for acute burns and reconstructive needs. Half of the unit capacity is dedicated to intensive care patients. The center’s nurses and doctors help heal people injured from fire, chemical agents, scalds and electrical burns.
The center was established in 1947 by Everett I. Evans, M.D. During Dr. Evans’ tenure as burn director, many advances in burn care were developed, including the first civilian intensive care unit and the first protocol for fluid resuscitation post-burn. Drs. Evans and Haynes also were early thought leaders in managing mass casualty events involving civilians. After Dr. Evans’ death, Boyd W. Haynes, M.D., directed the burn center for 36 years. Dr. Feldman became director in 2011.
“There’s a lot of people here who are passionate about burn care, who want to help people and have put extra time in to train and to learn how to use special products and how to treat these wounds and so much more,” Dr. Feldman said. “It’s something that takes a lot of time and a lot of training. And it just takes a passionate group of people to make it work.”
The future of burn care is only limited by our imagination, and our desire to make burn care better.
Michael Feldman, M.D., medical director, Evans-Haynes Burn Center
In addition to the direct nursing teams and physicians, Dr. Feldman credits a host of specialists who are critical for successful patient outcomes. This includes radiologists, surgical techs, lab personnel, environmental services staff, infection specialists and personnel in the supplies and equipment departments. The environmental services staff are critical to preventing infection, given the high risk. Frequent cleaning and special protocols with ultraviolet lights help mitigate the risk of multidrug-resistant bacteria and keep patients safe. Around every corner of the ward there is easy access to hand sanitizer, which staff use noticeably more frequently when roaming the floor.
“When we think of burn care, we are often thinking of our front-line workers and they are so important, but just as important are those who work tirelessly behind the scenes,” said Beth Broering, trauma and burn program manager. “Without their unrivaled commitment to our patients and their work in the environment, we would not have the outcomes we have.”
“On average, we’ve been able to reduce length of stay and to improve rates of healing because we offer the newest technology in terms of skin substitutes,” Dr. Feldman said. “Charlie Xavier’s story [see Patient Perspective] is a great example of how our abilities can help patients achieve outcomes even beyond our expectations and estimates.”
The burn center space has been specifically designed to optimize care.
“Patients who lose skin due to burns often must be kept in warmer rooms to ensure their safety and recovery,” Dr. Feldman said. “You can imagine if you don’t have skin, you get cold very quickly and that can cause lots of problems.”
Keeping rooms at temperatures in the upper 80s is one element that makes burn care unique. Traditional burn treatment is also intensive for the patient and often involves using skin grafts, a procedure in which providers take healthy skin from one part of the body and move it to cover skin that’s damaged or missing. But in extreme cases, there isn’t enough healthy skin to help repair a burn wound.
When this happens, providers look for a piece of healthy skin that can be sent off to a lab where they will grow new skin. This process can take weeks and must take place over and over again until they get enough skin to heal the wounds. It takes patience, dedication and passion to help those whose lives have been upended and scarred by flames.
“Taking care of burn patients is the ultimate honor as a surgeon,” Dr. Feldman said. “You care for adults and children, and then you get to follow these patients for sometimes their entire life and watch them grow up if they’re children. You become a part of the family.”
Old, but Bold: Patient-Centered Research
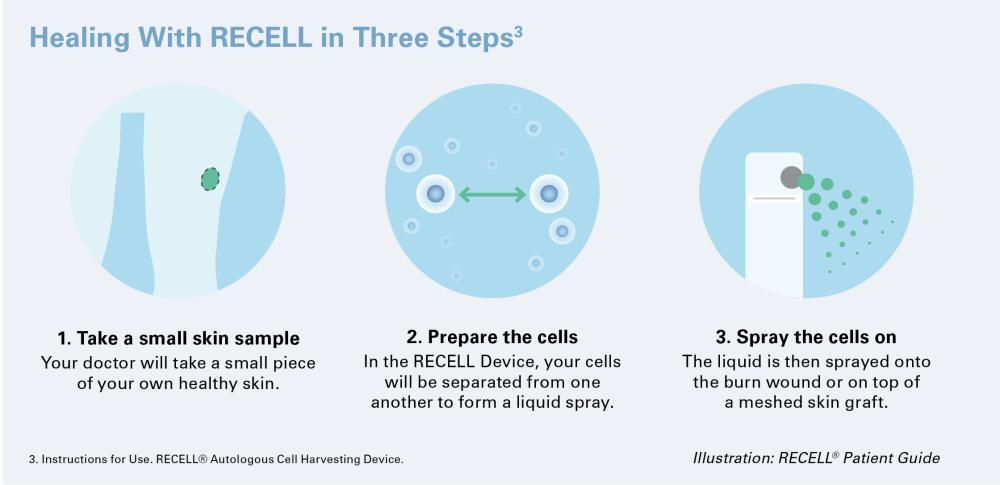
Evans-Haynes continues to have a robust level of research aimed at improving patient outcomes. Newer technology like RECELL® can speed up the healing process. Providers can take a smaller piece of skin and process it in the operating room without ever having to send it out to a lab. RECELL is an innovative, clinically proven approach for thermal burn treatment that VCU Health helped test in adult and pediatric care. Some of the early trials were so successful, they ended early.
“Evans-Haynes was part of the burn centers who participated in the development of this product, and it really is quite amazing,” Dr. Feldman said. “There is no downtime, no waiting for the lab to send the skin back to you. I can process it in the operating room and then apply it right away — this is unheard of.”
The process starts by taking a small sample of the patient’s skin and putting it into a device that mixes the sample with a special enzyme mixture that separates out the individual skin cells responsible for skin proliferation, healing and pigmentation. The cells are put into a suspension that is then sprayed on a wound. A 1-square-centimeter sample can be used to cover 80 square centimeters of wound.
The technology is incredibly effective in reducing the amount of donor skin needed to be harvested to use in grafting. It can help decrease pain and scarring of wounds. With fewer surgical procedures and less downtime, it reduces the time it takes patients to heal and recover and allows patients to leave the hospital sooner.
Dr. Feldman sees the evolution of care going even further through some basic science research, including projects aimed at figuring out how to reduce or stop wound conversion, or when over time a second-degree burn intensifies to a third-degree burn or becomes infected. In the not-too-distant future, burn care could entail using stem cell technology or 3D printing to create skin grafts using a patient’s genetic material.
“The future of burn care is only limited by our imagination,” Dr. Feldman said, “and our desire to make burn care better.”
Research also has focused on addressing burnout among care providers. Wound care can be emotionally draining for caregivers. To prevent infection requires a frequency of cleaning and dressing the burn wounds, which is both painful and necessary to prevent complications once the skin’s outer layer of protection has been compromised through injury.
A recent project led by nurse clinician Tiffany Lord, D.N.P., developed a virtual reality program to help reduce the emotional toll that wound care has on care providers. Patients could immerse themselves in a relaxing scene using virtual reality goggles while receiving wound care. Later, Dr. Lord learned her colleagues on the nursing staff also found the technology helpful on breaks from their everyday work, especially during the added stress of the pandemic.
What’s Next?
As VCU Health’s burn center prepares to celebrate its 75th year, its longevity has only strengthened resolve among the team to continue to pursue promising research that can help ease burn patient suffering or accelerate healing. Equally important is ensuring that tomorrow’s patients will have trained providers who can provide specialized care to burn victims.
Even today, the need has been growing. During the COVID-19 pandemic, Evans-Haynes saw a 40% increase in its patient census over the previous two years, including a 12% increase in pediatric patients as families stayed home during lockdowns.
“We have the only burn fellowship in the Commonwealth,” Dr. Feldman said. “We are the only outfit training future burn surgeons in Virginia, which is impressive, but also very necessary with an increasing number of burn patients. We need more people who know what they’re doing and how to take care of burns.”
Dr. Feldman also appreciates firsthand the importance of mentorship in inspiring the next generation of burn care specialists. An invitation to scrub in on a case during his time as a medical student on the MCV Campus is what ignited Dr. Feldman’s passion for burn care when observing and assisting on a case involving an artificial skin product.
“It’s all about the people you meet early in your career,” Dr. Feldman said. “I met mentors who were very enthusiastic and good teachers, and they molded me into my current career. They were academic surgeons at their heart, and I knew that’s what I wanted to be, too. My hope is that we can strengthen our fellowship program into the first American Burn Association-verified fellowship program in Virginia, continue to evolve our offerings, along with making sure we uphold the highest standard of care to our patients while they’re most vulnerable.”
If you are interested in supporting the work of the Evans-Haynes Burn Center at VCU Health, contact Nathan Bick, senior director of development in the Office of Medical Philanthropy and Alumni Relations, at 804-827-0387 or nathan.bick@vcuhealth.org.
PATIENT PERSPECTIVE
Read how Charlie Xavier beat the odds with the help of the Evans-Haynes Burn Center.
Make an Impact
Support the continued excellence of the burn center.
