A Whole-Body Experience

By A.J. Hostetler, VCU Stravitz-Sanyal Institute for Liver Disease and Metabolic Health
Thanks to a full embrace of research and patient care surrounding a sometimes overlooked organ, the VCU School of Medicine is making discoveries that could dramatically improve lives for millions of people around the world.
The liver plays a role in more than 500 vital processes for the body — from filtering toxins to assisting with digestion, immunity and storage of vitamins.
New research from campus also shows that the prevalence of certain forms of dementia caused by scarring and inflammation in the liver may be reversible with readily available treatments.
“The liver controls the health of all of the other organs,” said Arun Sanyal, M.D., director of the Stravitz-Sanyal Institute for Liver Disease and Metabolic Health and chief of the Division of Gastroenterology, Hepatology and Nutrition at the VCU School of Medicine. “So very simply put, the liver is the driver of human health and well-being.”
The VCU Stravitz-Sanyal Institute is a global leader in the quest to better treat liver issues, advance the scientific understanding of overall metabolic health and identify the liver’s links to diseases throughout the body. The institute was created in 2022 after a historic $104 million gift from R. Todd Stravitz, M.D., and his family’s Barbara Brunckhorst Foundation. It remains the largest publicly shared gift for liver research in U.S. history.
“Our vision is really to transform the lives of people with liver disease through innovation and by training the next generation of investigators,” Dr. Sanyal said.

The vision is now evident in the research output and insights being gained by researchers and clinicians here in Richmond. Dr. Sanyal was among five faculty members at the institute who were recently named in the top 2% of the most influential scholars and scientists worldwide in career rankings compiled by Stanford University and analytics firm Elsevier based on citation metrics, co-authorship and other factors that ensure a diverse roster and representation of researchers. Joining him on that list are Dr. Stravitz, institute co-founder; Richard Sterling, M.D., chief clinical officer; Saul Karpen, M.D., Ph.D., chief scientific officer; and Jasmohan Bajaj, M.D.
In just two years, the collective progress made in advancing scientific understanding has been impressive and swift. The institute has also been developing and training a global network of researchers and clinicians to ensure the broadest reach for its insight into care.
UNRAVELING THE MIND-LIVER CONNECTION
One of the most intriguing discoveries from the Stravitz-Sanyal Institute includes research demonstrating that around 13% of individuals diagnosed with dementia may suffer instead from reversible cognitive decline caused by advanced liver disease.
This important link between dementia and liver health emphasizes the importance of screening patients for potentially treatable contributors to cognitive decline.
Jasmohan Bajaj, M.D., gastroenterologist, the Stravitz-Sanyal Institute and the Richmond VA Medical Center
Researchers at the VCU School of Medicine and the Richmond Veterans Affairs Medical Center published these findings recently in the American Journal of Medicine. They included the additional analysis of nonveteran patients that corroborated and extended the research group’s earlier work. The results showed that about 10% of U.S. veterans diagnosed with dementia may suffer instead from cirrhosis, and those earlier findings appeared in the journal JAMA Network Open.
It can be difficult for physicians to differentiate dementia from hepatic encephalopathy, which is the cognitive decline caused by cirrhosis. If it is undetected, patients will not receive treatment that can reverse or halt the impairment. Hepatic encephalopathy is a nervous system disorder brought on by cirrhosis, an advanced form of liver disease in which patients experience severe scarring of the liver.
When the liver doesn’t work properly, toxins build up in the blood. These toxins can travel to the brain and affect brain function, leaving patients confused or delirious. Widely available medications can readily rid the body of toxins and reverse this condition, but without treatment, patients can lapse into a coma or die.
The VCU-VA analysis suggests that physicians treating veteran or nonveteran patients with dementia — even without a cirrhosis diagnosis — should consider assessing them for liver disease. Identifying cirrhosis early on may point to reversible causes of cognitive impairment, potentially improving the lives of these patients.
“This important link between dementia and liver health emphasizes the importance of screening patients for potentially treatable contributors to cognitive decline,” said the study’s corresponding author, Dr. Bajaj, a gastroenterologist with the Stravitz-Sanyal Institute and the Richmond VA Medical Center.
In their publication of results from the VA study, researchers said that they believed the findings would apply to nonveterans with dementia, but that further research was needed. The subsequent study also sought to provide additional data by examining health records of nearly 69,000 nonveteran patients diagnosed with dementia between 2009 and 2019.
Almost 13% of the patients with dementia had high scores that are used to estimate the level of scarring of liver tissue, meaning they were very likely to have cirrhosis.
Dr. Bajaj said it should not be difficult to incorporate liver assessments into routine care for patients, as their risk for liver disease can be easily evaluated with an initial, noninvasive screening tool called the FIB-4 index.
“Early detection of liver issues, which can contribute to the treatable cognitive decline known as hepatic encephalopathy, in those with dementia could help ensure that patients get access to targeted and appropriate therapies,” Dr. Bajaj said.
DEVELOPING SCORING FOR SCARRING
The FIB-4 score is recommended by leading liver, gastroenterology and endocrinology associations as a first-line test to screen for liver scarring, or fibrosis. It is based on multiple measurements, including age, and was developed by Dr. Bajaj’s VCU Health colleague and co-author on the new study Dr. Sterling, the chief clinical officer of the Stravitz-Sanyal Institute.
Dr. Bajaj’s interest in the connection between dementia and cirrhosis was sparked by the cases of two older veterans who were thought to have dementia and Parkinson’s disease but whose symptoms dramatically improved after being treated for hepatic encephalopathy. About 30% of veterans suffer from some form of liver disease, and in 2023, it was estimated that about 8% of U.S. veterans with cirrhosis had dementia.
In the VCU study published in JAMA Network Open, researchers reviewed medical records of 177,422 U.S. veterans diagnosed with dementia, but not cirrhosis, between 2009 and 2019. It showed that 10.3% of veterans with dementia had high FIB-4 scores and were very likely to have cirrhosis.
Factors that increase the risk of cirrhosis include older age, being male, congestive heart failure, viral hepatitis, alcohol use and other health conditions. The new findings among nonveterans were unexpectedly higher than those for veterans, Dr. Bajaj noted.
“The 13% rate we found in nonveterans was surprising in that it was higher than we found among veterans, who tend to be older, less diverse and more male. But ultimately, it confirms and extends the results in a database more reflective of the U.S. population,” said Dr. Bajaj, who has spent the past several years focusing on hepatic encephalopathy and the gut-brain axis and helped author the new findings on nonveteran patients published in the American Journal of Medicine. “The next step is to ensure that health care providers are made aware of this potential overlap between dementia and hepatic encephalopathy, which is treatable.”
CONFRONTING A GLOBAL CHALLENGE: FATTY LIVER DISEASE
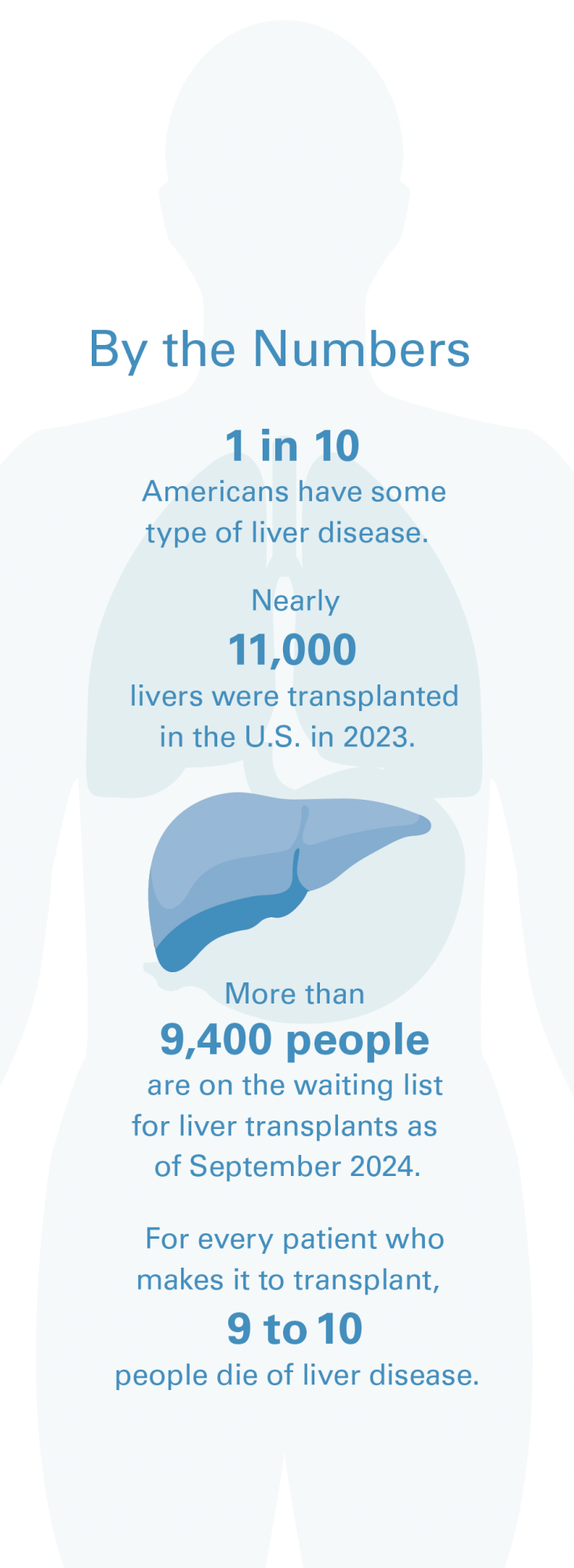 Liver-related dementia is just one of the many issues caused by a failing liver that institute researchers are working to address. Among some of the most significant liver conditions is fatty liver disease, also known as steatotic liver disease, which develops when the body begins storing excess fat in the liver. This doesn’t always cause problems for people, but when it does, the buildup of fat can cause inflammation and damage. Because of the liver’s crucial role in helping the body process nutrients, remove toxins and build key proteins, the disease can precipitate multiple medical issues. The condition affects as many as 15 million people in the U.S. alone.
Liver-related dementia is just one of the many issues caused by a failing liver that institute researchers are working to address. Among some of the most significant liver conditions is fatty liver disease, also known as steatotic liver disease, which develops when the body begins storing excess fat in the liver. This doesn’t always cause problems for people, but when it does, the buildup of fat can cause inflammation and damage. Because of the liver’s crucial role in helping the body process nutrients, remove toxins and build key proteins, the disease can precipitate multiple medical issues. The condition affects as many as 15 million people in the U.S. alone.
The advanced stage of fatty liver disease is called metabolic dysfunction-associated steatohepatitis, or MASH, which is the leading cause of liver-related medical conditions and mortality. MASH affects approximately 6 to 8 million people in the U.S., and it is often associated with other health problems, such as high blood pressure, Type 2 diabetes, obesity and high blood fat levels.
The condition is closely linked to obesity and diabetes. That means that many people are gradually developing fatty deposits in their livers, which cause greater inflammation and can lead to serious organ disease and death if left unaddressed. Often, the warning signs come too late to reverse the damage. As it worsens, it can cause scarring, known as fibrosis, and can continue to advance to significant fibrosis or even cirrhosis, cancer and the need for a liver transplant.
“The liver is the only way you can get rid of extra cholesterol,” said Dr. Sanyal, the director of the Stravitz-Sanyal Institute. “Those who take statins are really taking a drug that works on the liver to lower cholesterol. The liver controls how the heart works, and it generates fuel and controls the supply of energy for all the body’s other organs. It’s complicated stuff.”
Researchers at the Stravitz-Sanyal Institute have been exploring multiple potential treatments, often collaborating with industry leaders investigating drug candidates. Most recently, Dr. Sanyal was a key investigator in the Phase 3 trial for resmetirom. Until the Food and Drug Administration approved resmetirom to treat fatty liver disease in March 2024, there were no approved drugs to treat the condition. The problem is so pressing that the FDA approved the resmetirom, now branded as Rezdiffra, under its accelerated approval pathway, which allows for earlier approval of drugs that treat serious conditions and address an unmet medical need.
Dr. Sanyal was a pivotal leader whose broader contributions to the field helped establish the pathway to this approval.
“This is a major milestone for our patients and for the field. MASH is a leading cause of liver-related morbidity and mortality,” Dr. Sanyal said. “With resmetirom approved, our patients with clinically significant scarring of the liver due to MASH will have access to an effective and approved therapeutic agent to reverse disease progression. As an investigator working on MASH, I congratulate Madrigal Pharmaceuticals and the communities of scientists and patients who participated in the treatment trials to make approved therapy for MASH a reality.”
Resmetirom became available for patients in April 2024 and is approved to treat MASH. The medication is intended for people with MASH whose livers indicate moderate to advanced fibrosis — when patients are on the cusp of cirrhosis. Additional drugs are undergoing clinical testing to treat patients whose fibrosis is less advanced and could possibly halt the scarring or even lessen the amount of fat in the patient’s liver.
Until Madrigal’s development of resmetirom, physicians treating MASH patients focused on managing the disease through weight loss from lifestyle changes such as a healthy diet and regular exercise. The newly approved medication targets a protein directly in the liver and reduces liver fat, inflammation and scarring.
Clinical trials found it can halt the progression of fibrosis or even reverse it. It’s intended to be used along with a healthy diet and exercise. Liver disease is often called “silent” because so many patients don’t feel any symptoms and their illness goes undiagnosed, but it is the ninth leading cause of death in the U.S. and is an increasing burden on health care systems globally. Patients with MASH, especially those with metabolic diseases like obesity or Type 2 diabetes, are at greater risk for adverse cardiovascular events and increased illness and mortality.
WHAT’S NEXT?
Researchers at the Stravitz-Sanyal Institute are working on a broad array of projects to improve overall liver health. One project seeks to measure the effect on liver scarring by a class of drugs known as glucagon-like peptide 1 agonists (GLP-1). Most people will know this type of drug by names like Ozempic, a medication developed to help regulate insulin in Type 2 diabetes patients that has also become popular to use off-label for weight loss.
Early studies, including several involving Dr. Sanyal, have suggested benefits for liver health. The drugs work by mimicking the actions of the GLP-1 hormone that stimulates production of insulin and have been shown to curb hunger. The better regulation of blood sugar and weight ultimately also benefit the liver’s health according to early studies at the center.
As the institute has grown, its roster of experts has deepened its bench strength. The chief scientific officer, Dr. Karpen, identified the first genetic variant to biliary atresia, a rare disease of the liver and bile ducts that occurs in infants. Juan Pablo Arab, M.D., who recently joined the institute, is a world leader in the study of alcohol-related liver disease, striving to advance early diagnosis and treatment strategies to improve patient outcomes. And the chief clinical officer, Dr. Sterling, not only developed the gold standard, noninvasive test for estimating fibrosis, but he is also an expert in hepatitis and liver disease in people living with HIV.
With this team of specialists, the liver institute broadens its areas of research expertise and hopes to create a sea change in the way the world understands the liver as the key to overall health.
“It has been a fantastic journey over the last few years creating this disruptive influence,” Dr. Sanyal said, “because it is only through disruption that we will transform medicine with transformed human health and the human state.”
If you would like to support research at the VCU Stravitz-Sanyal Institute for Liver Disease and Metabolic Health, please contact Nathan Bick, executive director of development in the VCU Office of Medical Philanthropy and Alumni Relations, at 804-827-0387, or ngbick@vcu.edu.
Support Liver Research
Make a gift to the Stravitz-Sanyal Institute for Liver Disease and Metabolic Health.