Michael Hindle, Ph.D., the Peter R. Byron Distinguished Professor in the VCU School of Pharmacy, and Worth Longest, Ph.D., a professor in the VCU School of Engineering are on their way to changing the way aerosol medications are delivered to the lungs. Their new approach may dramatically improve the amount of medication that reaches its target.
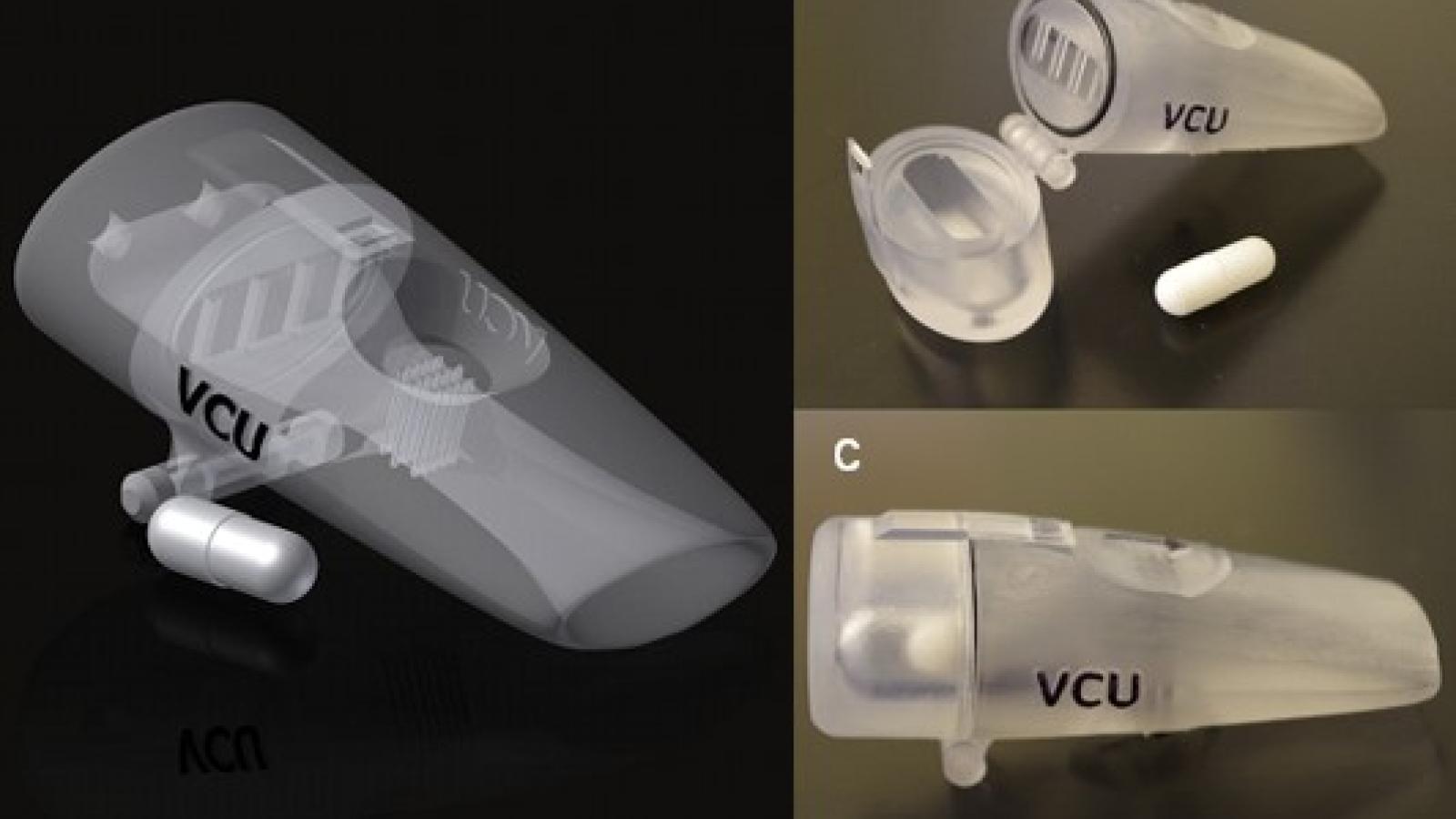
A dry powder inhaler developed by Drs. Hindle and Longest
The Right Place: How Two Researchers are Ensuring Medications Reach the Lungs
Making sure medications get to the right place in the body for optimal treatment is an ongoing concern in healthcare.
In aerosol treatments intended for the lungs, 60-90 percent of the medication is wasted and never reaches its target in adults. In infants, the numbers are even worse: 90-99 percent of the medication hits the back of the throat or deposits in the nasal cavity and goes no farther.
Michael Hindle, Ph.D., the Peter R. Byron Distinguished Professor in the VCU School of Pharmacy, and Worth Longest, Ph.D., a professor in the VCU School of Engineering, have been working together to solve the aerosol delivery problem, and they now believe that testing their novel strategy in humans will show the possibility of completely inverting current statistics, delivering very large percentages of medications that currently are wasted.
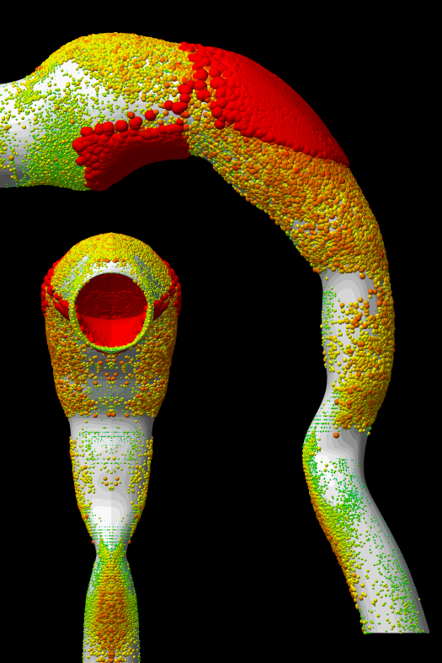
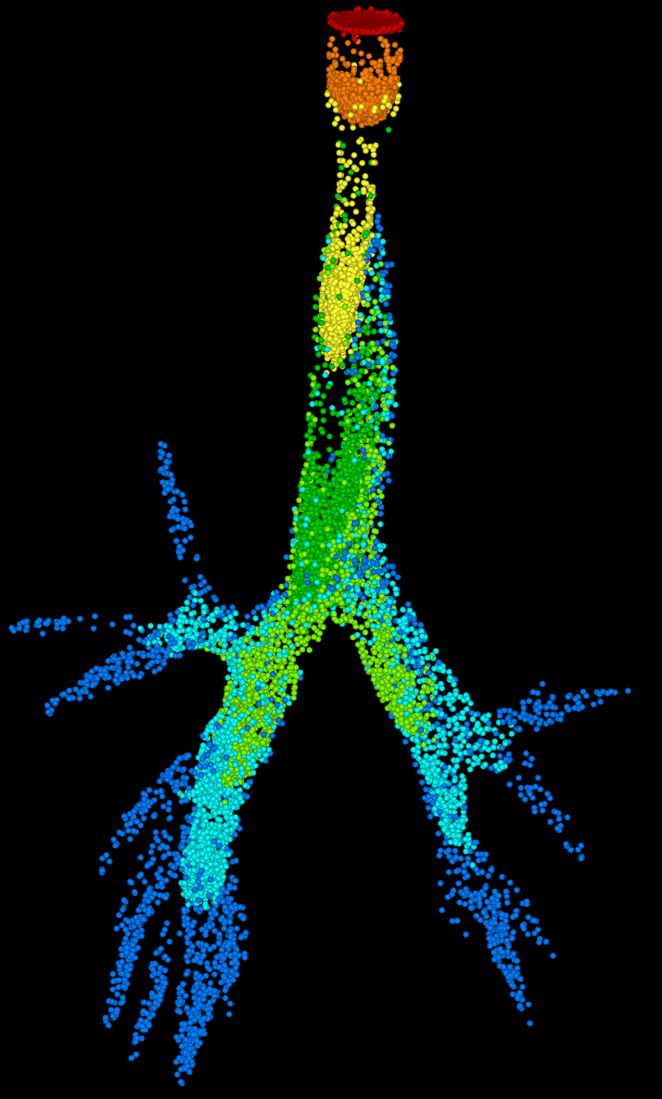
Their strategy is to reduce the aerosol medication size, allowing particles to slip easily through airways, past the throat or nasal cavity and into the lungs. Then, after reaching the lungs, the particles have been engineered to triple or quadruple in size, providing the momentum they need to deposit at the desired target site before they’re exhaled.
Drs. Hindle and Longest are pursuing three specific applications with their strategy.
The first application is a human proof-of-concept study in which they will deliver aerosols using the novel high-efficiency delivery technology they developed, and then measure waste/delivery rates. A $2.4 million National Institutes of Health grant renewal that they received in 2017 will enable them to take their technology out of the lab and on to human testing.
The second application is the development of a pediatric dry powder inhaler for delivery of antibiotics to children with cystic fibrosis. There are currently no inhalers specifically developed for children, and children who need inhaled medication spend many hours on nebulizers because of inefficient delivery methods.
Drs. Hindle and Longest have data from a model for this project that show less than 1 percent of the dose from their inhaler was lost on the back of the throat, meaning 99 percent reached the lungs. They are the two co-principal investigators on a five-year, $2.5 million NIH grant that will support them in completing this project.
The third application is delivering lung surfactants to premature babies in neonatal intensive care units. The current standard of care when babies lack these surfactants is to intubate them and squirt liquid down their lungs. Dr. Hindle said this is a great opportunity to use some of his technology to deliver surfactants less invasively as an aerosol via a nasal canula, which would remove the need to intubate.
As the Peter R. Byron Distinguished Professor in the VCU School of Pharmacy, Dr. Hindle’s position and the research described above are supported by an endowed fund. Endowments are extremely important to the quality of our campus programs, as they provide long-term financial stability regardless of government funding and changes in the economy. Donors can create an endowment to support students, faculty, research or other programs across the campus.
To learn more about named endowed funds, visit our endowed fund page. To learn more about other ways to give, such as planned giving, major gifts and tributes or memorials, visit our giving page.
A longer version of this story and others that highlight life-saving patient care, research and education on the MCV Campus at VCU Health appeared in the inaugural issue of NEXT magazine. To read NEXT online, click here. To sign up to receive your own copy of NEXT, click here.